 The term pericardial window refers to a surgical procedure of the heart that involves making an opening within the pericardium which is the membrane sac enclosing the heart. In a pericardial window procedure, the incision created in the pericardium relieves pressure caused by fluid around the heart, something known as pericardial effusion. In some cases, the surgeon may also place a tube which drains extra fluid following the surgery to help the heart be able to effectively pump again. A surgeon may use a pericardial window to look at possible biopsy sites as well.
The term pericardial window refers to a surgical procedure of the heart that involves making an opening within the pericardium which is the membrane sac enclosing the heart. In a pericardial window procedure, the incision created in the pericardium relieves pressure caused by fluid around the heart, something known as pericardial effusion. In some cases, the surgeon may also place a tube which drains extra fluid following the surgery to help the heart be able to effectively pump again. A surgeon may use a pericardial window to look at possible biopsy sites as well.
What Is Pericardial Window?
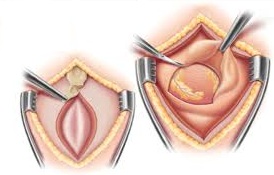
The pericardial window, also referred to as subxiphoid pericardiostomy, is typically done when fluid accumulates around the heart. During the procedure, the surgeon creates an opening to drain the fluid in the pericardium.
- The Procedure of Pericardial Window
The procedure begins by putting the patient under anesthesia. The window will usually be placed through the ribs along the patient’s left side or below the sternum. The surgeon makes a small incision in the pericardium so excess fluid can get released into the patient’s abdomen. Later, this fluid will be harmlessly absorbed into abdominal tissue.
- Why Is Pericardial Window Performed?
Patients usually have a pericardial window because of pericardial effusion. The pericardium surrounds the heart and is a sac. It typically holds the right amount of fluid to lubricate and cushion the heart muscle. Fluid may build up for numerous reasons, including injury, renal disease, cancer and viral infection. When too much fluid is in the pericardium, the pressure will make it difficult for a patient’s heart to pump normally. This pericardial effusion can lead to painful breathing, shortness of breath, a rapid heartbeat, dizziness and fainting. If it isn’t treated, pericardial effusion may cause heart failure or even death.
Should I Have a Pericardial Window?
As a minimally invasive, therapeutic or diagnostic procedure, the pericardial window is typically suggested in the following cases:
- Pericardial effusion with anxiety, shortness of breath, palpitations, hoarseness, cough, lightheadedness, pressure or discomfort or chest pain.
- Effusions or delayed haemopericardium (blood within the pericardial sac) after cardiac surgery
- Chylopericardium (a milky fluid with fat and lymph accumulating in the pericardium)
- Benign effusions which recur following aspiration
- Pericarditis (pericardium inflammation)
- Purulent pericardial effusion (an infection of the pericardial space)
- Hemodynamically stable (when the blood pressure is sufficient to bring blood to all areas of the body), but undiagnosed pericardial effusion
In some cases, the pericardial window will be contraindicated, such as in situations with a concomitant cardiac surgery requiring an incision that separates the chest bone known as a sternotomy.
Talk to your health care team about the possible pericardial window complications, risks, and benefits.
What to Expect from Pericardial Window
1. An IV will be inserted in your arm so it can give you medications during and after the procedure. Your pain will be controlled via medications through the IV or oral ones. The surgery itself takes place under general anesthesia.
2. During recovery, your care provider will ask you to walk around your unit multiple times daily. Many patients return to their homes in two days, but this varies based on the principle disease.
3. There is always a risk of complications associated with treatment and diagnostic procedures. Although these issues are rare, it is important to be informed before the procedure. The potential pericardial window complications are similar to those associated with other procedures and include:
- Recurrence of the pericardial effusion which may need further operation
- Arrhythmia (heartbeat that is irregular)
- Heart attack
- Cardiac arrest
- Bleeding
- Infection
Other Ways to Treat Pericardial Effusion
1. Medication
In cases when you don’t have tamponade (a decrease in the function of your heart due to exerted pressure) and there isn’t an immediate threat of one, it is common for doctors to prescribe medication to reduce pericardium inflammation.
Potential medications your doctor may prescribe include Colchicine, ibuprofen (Advil, Motrin IB), indomethacin (Indocin), NSAIDs (non-steroidal anti-inflammatory drugs) and aspirin. A corticosteroid like prednisone may also be prescribed for patients who don’t respond positively to other medicines or those who experience a recurring pericardial effusion following a successful treatment.
2. Pericardiocentesis
Your doctor may do a procedure known as pericardiocentesis which involves using a needle to get into the pericardial space before draining fluid from your pericardium with the help of a catheter (small tube). Most of the time, the catheter is left in place for several days following the procedure, allowing it to keep draining the pericardial space and prevent fluid from beginning to build up again.
3. Intrapericardial Sclerosis
Intrapericardial sclerosis is another possible procedure that serves as an alternative to the pericardial window. It involves injecting a solution into the area that separates the pericardium’s two layers and this will effectively seal the layers together. Intrapericardial sclerosis is an option in the case of effusion due to cancer or recurring pericardial effusion.
4. Pericardiectomy
Your doctor may suggest a pericardiectomy which is the process of surgically removing part of the pericardium or the entire organ. The heart is able to function without the pericardium, but this procedure is usually done when pericardial effusion recurs despite draining with a catheter.